[box type=”bio”] What to Learn from this Article?[/box]
While dealing with patients with extensive skeletal lesions and pathological fractures, secondaries due to adenocarcinoma elsewhere should be kept in mind along with other probabilities such as multiple myeloma. With the increasing availability of imaging and invasive diagnostic techniques, an individualized treatment protocol needs to be adapted.
Case Report | Volume 7 | Issue 2 | JOCR March – April 2017 | Page 44-47| Vanamali B Seetharamaiah, B Sunil, M K Padmanabha, N Sparsha. DOI: 10.13107/jocr.2250-0685.744
Authors: Vanamali B Seetharamaiah[1], B Sunil[1], M K Padmanabha[1], N Sparsha[1]
[1] Department of Orthopedics, Bangalore Medical College and Research Institute, Victoria Hospital, KR Road, Bengaluru, Karnataka, India.
Address of Correspondence
Dr. Vanamali B Seetharamaiah,
Bangalore Medical College and Research Institute, Victoria Hospital, KR Road, Bengaluru – 560002, Karnataka, India.
E-mail: vanamaliseetharam@gmail.com
Abstract
Introduction: Pathological fractures due to secondaries in the bone are common with carcinoma of lung, breast, prostate, and in multiple myeloma. Multiple pathological fractures after a trivial fall, indicating metastases warrants detailed investigations for the search of primary. Skeletal secondaries should be strongly suspected in addition to obvious diagnosis of multiple myeloma in such cases.
Case Report: We report a case of pathological fractures at multiple sites: The vertebral column, proximal shaft of femur, and contralateral fracture neck of femur. This patient presented with typical features of multiple myeloma, but on complete evaluation was found to be due to extensive metastases in the bones secondary to adenocarcinoma, the primary site of which remained unknown, despite extensive search and evaluation, making it a case of carcinoma of unknown primary.
Conclusion: While dealing with patients with extensive skeletal lesions and pathological fractures, secondaries due to adenocarcinoma elsewhere should be kept in mind along with other probabilities such as multiple myeloma.
Keywords: Pathological fractures, carcinoma of unknown primary, multiple myeloma.
Introduction
Multiple pathological fractures after a trivial fall, indicating metastases warrants detailed investigations for the search of primary. Multiple myeloma is an obvious diagnosis in majority of these cases. However, other causes such as secondaries should be kept in mind. We present a case with X-ray and other imaging features, positive urinary Bence Jones proteins and serum electrophoresis suggestive of multiple myeloma, but histopathology of bone marrow biopsy revealed adenocarcinoma, the primary site of origin of which remained unknown despite extensive search. This was a case of carcinoma of unknown primary (CUP).
Case Report
A 65-year-old woman presented with pain in the right hip with a history of a trivial fall and inability to bear weight on the right lower limb since the fall. She was investigated after initial clinical assessment. History revealed diffuse bone pain, loss of appetite, loss of weight by 25% over the past 3 months, and Type-II diabetes mellitus. Anterior joint line tenderness was elicited with painful and restricted range of active movements of the right hip, suggestive of fracture of the neck of femur. It was confirmed by X-ray. Patient was ambulatory earlier to this event. Her age and the severity of the injury sustained after a trivial fall indicated a detailed clinical evaluation for the search of primary. Initial X-rays of the pelvis, proximal femur, and skull showed extensive lytic lesions indicating pathological fractures, suggestive of multiple myeloma. While other investigations were suggestive of multiple myeloma, not all investigations were in line with the diagnosis of multiple myeloma. S.CRP = 94.48 mg/L; erythrocyte sedimentation rate (ESR) = 110 mm/1st h; lactate dehydrogenase (LDH) = 697U/L; Bence Jones proteins in urine-positive; protein electrophoresis: “M” spike in the beta region. X-rays showed multiple punched out, lytic, sharply demarcated lesions without surrounding reactive sclerosis in the skull, pelvis, femur and spine, and mimicking multiple myeloma (Fig. 1, 2, 3, 4).Alkaline phosphatase = 563 U/L; serum immunofixation: Negative for monoclonal gammopathy. Ultrasonography abdomen showed minimal endometrial and pouch of Douglas collection.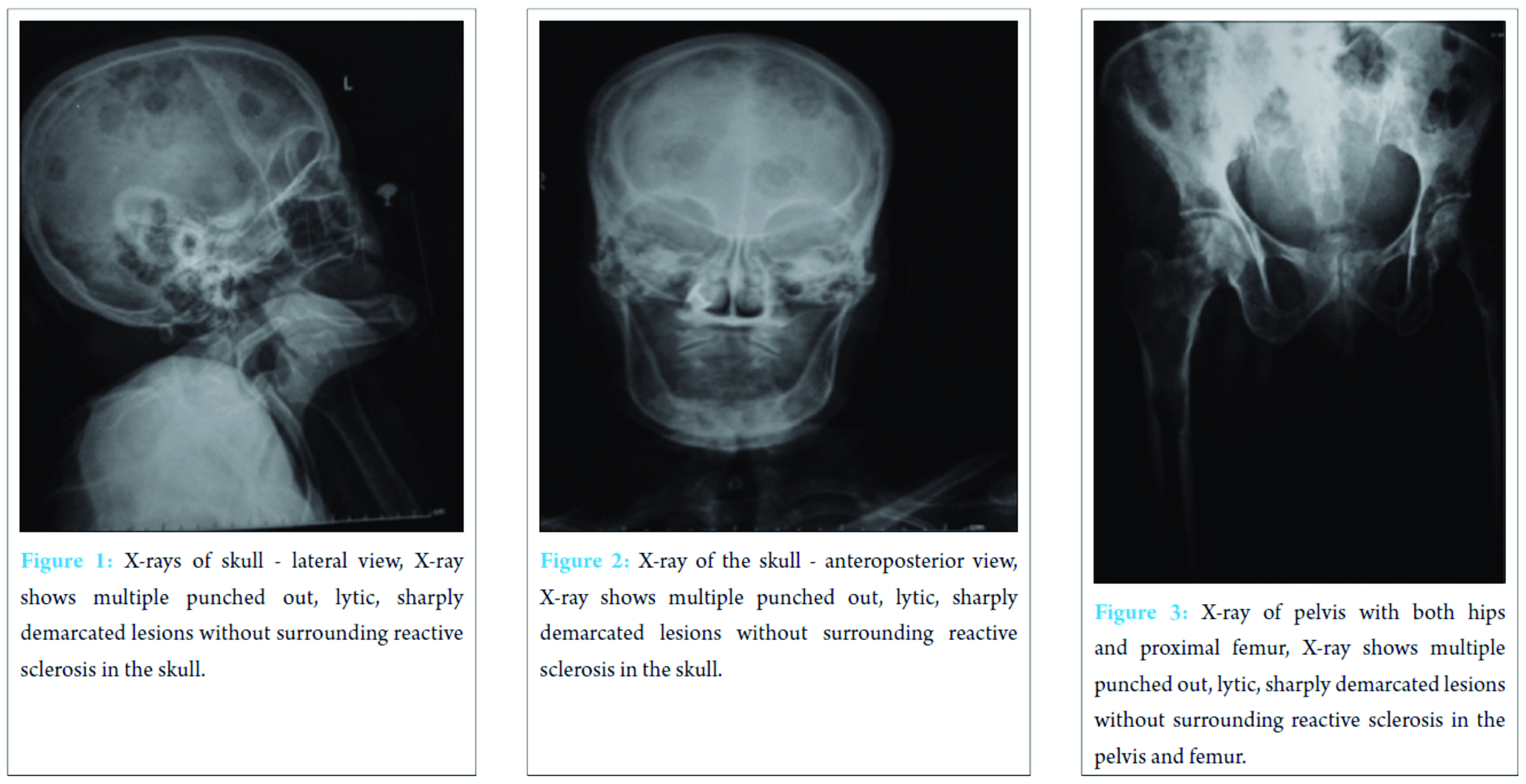
Magnetic resonance imaging (MRI) spine, pelvis with both hips and femur revealed pathological fracture of left proximal femur, fracture of the neck of right femur with multiple T1 hypo, short-TI inversion recovery (STIR) hyperintense foci diffusely scattered throughout sacrum, pelvic bones, and bilateral femoral heads and shafts (Fig. 5 and 6).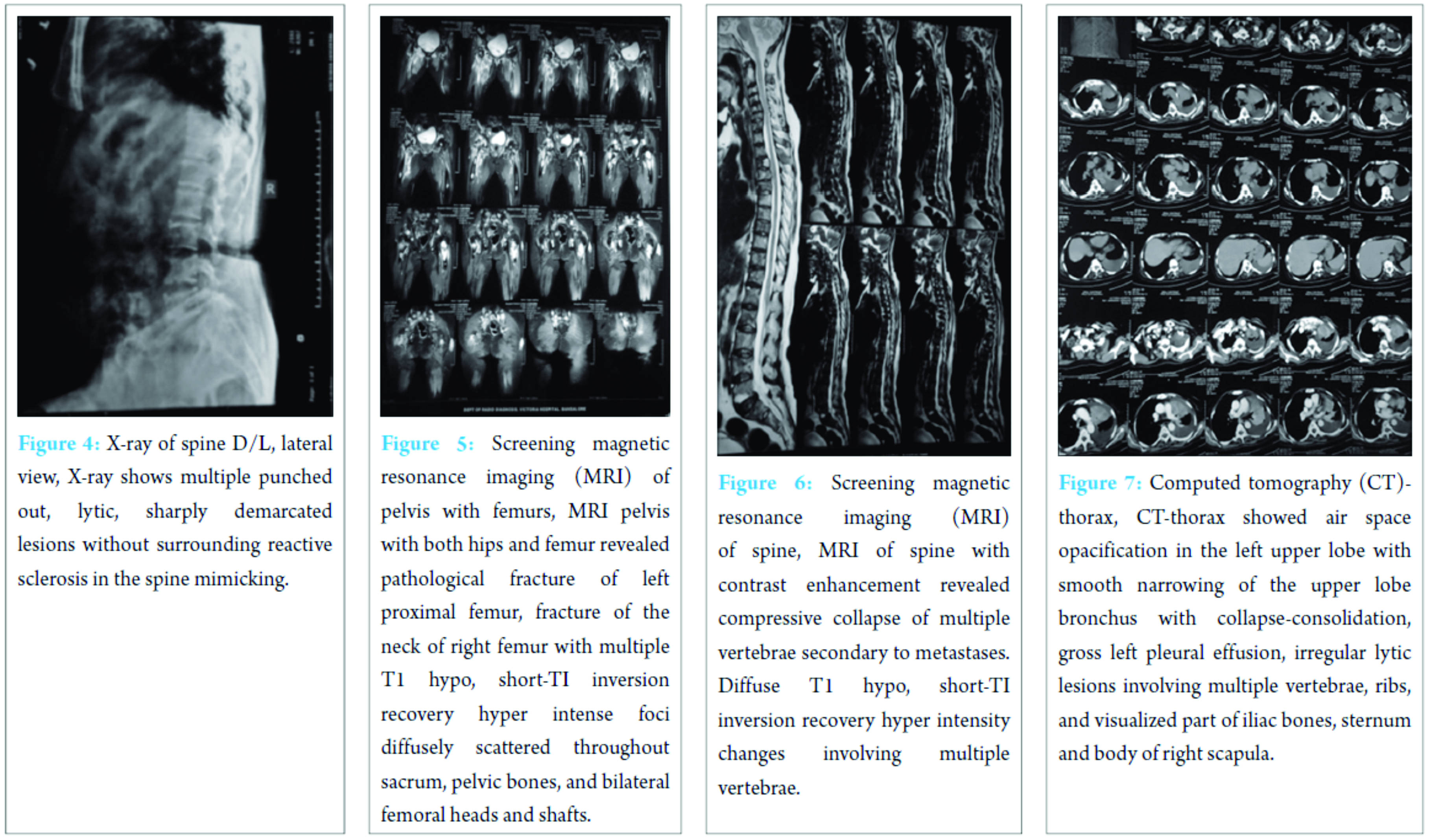
MRI of spine with contrast enhancement revealed compressive collapse of multiple vertebrae secondary to metastases. Diffuse T1 hypo, STIR hyperintensity changes involving multiple vertebrae suggestive of metastases. Computed tomography (CT)-thorax showed air space opacification in the left upper lobe with smooth narrowing of the upper lobe bronchus with collapse consolidation, gross left pleural effusion, irregular lytic lesions involving multiple vertebrae, ribs and visualized part of iliac bones, sternum and body of right scapula suggestive of metastases, or multiple myeloma (Fig. 7). On pleural fluid cytology, straw-colored fluid with predominantly lymphocytes and occasional mesothelial cells without malignant cells was reported. Bone marrow aspiration biopsy from the iliac crest showed evidence of metastatic deposits favoring adenocarcinoma after histopathology (Fig. 8 and 9). Biopsy from the site of the lesion procured by trochar under fluoroscopy showed features of metastatic secondaries suggestive of adenocarcinoma (Fig. 10).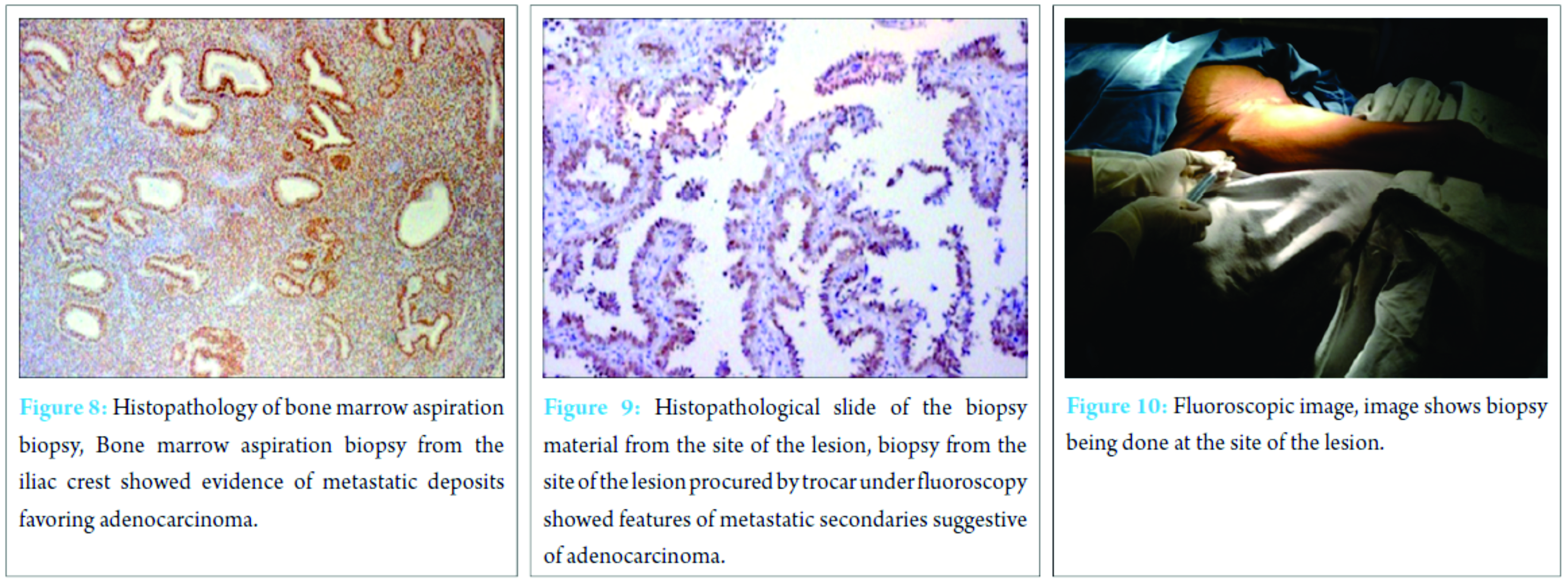
Intensive search for the primary including the evaluation of breast, bronchus, and lung, gastrointestinal and gynecological examination with endometrial biopsy were negative for evidence of malignancy.
Discussion
Bone is the third most common site for distant metastases from adenocarcinoma, second only to the lung and the liver [1]. Bone metastases were the first presentation of carcinoma in 23 percent of 429 previously undiagnosed patients [1]. In this case, clinical features, X-rays of skull and spine, contrast-enhanced MRI-scan, raised ESR, raised LDH, Bence Jones proteins in urine, and M-spike in the beta region on serum protein electrophoresis were suggestive of multiple myeloma. Raised serum alkaline phosphatase, minimal or no changes in the blood chemistries, normal renal functions, normal serum calcium, and histopathological features of adenocarcinoma on bone marrow biopsy were for a consideration of diagnosis of CUP. Raised LDH suggests high rate of cell death in malignant tumors along with the formation of new cells or multiple fractures. Heat test for Bence Jones proteins is a useful clinical test. However, one must be aware of false-positive and false-negative results [2]. Geschickter and Copeland from their own experience and review of literature collected 26 cases of Bence Jones proteinuria in diseases other than multiple myelomatosis [3]. Nine of these had skeletal metastatic tumors. Copeland reported three cases of carcinoma of the breast with skeletal metastases in which Bence Jones proteinuria was demonstrated [4]. Raised serum alkaline phosphatase could be accounted to multiple fractures. The chest X-ray and CT-thorax findings could be due to tuberculosis which got flared up in an immunocompromised state. Hingmire et al., suggested that multiple myeloma can coexist with a second carcinoma. In 5 cases out of 443, second neoplasm having coexisting malignancies was reported [5]. In our case, plasma cells were scanty histopathological, refuting a diagnosis of multiple myeloma, although other findings favor a diagnosis of the same. Although “M” spike in the beta region and raised beta-2 microglobulin levels on serum protein electrophoresis justify the diagnosis of multiple myeloma, serum immunofixation yielded negative results for monoclonal gammopathy denying the diagnosis of multiple myeloma sparing adenocarcinoma for the final diagnosis. CUP is a biopsy proven malignancy for which the anatomic site of origin remains unidentified after an intensive search [6]. CUP is one of the ten most frequently occurring cancers worldwide, accounting for approximately 3-5% of all cancers. Mean survival rate of CUP is 6-10 months [6]. Hypothesized that primary tumor either regresses after seeding the metastases or that the primary has been contained or eliminated by the natural defenses of the body, CUP may represent a specific malignant event that results in increase in metastatic spread or survival relative to primary [6]. Aruna et al. held that there is a possibility that the bone marrow serves as a “sanctuary” to protect metastatic breast cancer cells. They emphasized that a thorough work-up is necessary to come to a specific diagnosis in osteolytic lesions as a metastatic malignancy can mimic multiple myeloma or multiple myeloma can be camouflaged by metastatic deposit [7]. Among the metastatic adenocarcinomas, breast, lung, and prostate malignancies happen to be the most common primary sites of origin [8]. An extensive search with investigations for the primary site including endometrial biopsy, imaging of chest and abdomen did not reveal the primary, leading to the final diagnosis of CUP.
Conclusion
While dealing with patients with extensive skeletal lesions and pathological fractures, secondaries due to adenocarcinoma elsewhere should be kept in mind along with other probabilities such as multiple myeloma. With the increasing availability of imaging and invasive diagnostic techniques, an individualized treatment protocol needs to be adapted.
Acknowledgments
The authors would like to acknowledge the Department of Pathology, BMCRI for their support.
Clinical Message
CUP should be considered as a differential diagnosis in elderly patients with multiple skeletal lesions.
References
1. Aaron AD. Treatment of metastatic adenocarcinoma of the pelvis and the extremities. J Bone Joint Surg Am 1997;79(6):917-932.
2. Perry MC, Kyle RA. The clinical significance of Bence Jones proteinuria. Mayo Clin Proc 1975;50(5):234-238.
3. Geschickter CF, Copeland MM. Multiple myeloma. Arch Surg 1928;16:807-863.
4. Copeland MM. Skeletal metastases arising from carcinoma and sarcoma. Arch Surg 1931;23:581-654.
5. Hingmire S, Hingmire S, Bakshi A, Gujral S, Badwe R, Nair R. Multiple myeloma mimicking bone metastases in a patient of carcinoma breast. Indian J Med Pediatr Oncol 2008;29(1):53-55.
6. Varadhachary GR, Abbruzzese JL. Carcinoma of unknown primary. Harrison’s Principles of Internal Medicine. 18th ed. Ch. 99. New York: McGraw-Hill; 2001. p. 821.
7. Aruna L, Manimekhala P, Rahman S, Lavanya M, Sumanth D. Metastatic breast carcinoma with multiple osteolytic lesions-a diagnostic dilemma. J Evol Med Dent Sci 2014;3(2):322-325.
8. Basheer A, Daniel J, Padhi S. Compressive myeloradiculopathy from bony metastases as the initial presentation of poorly differentiated adenocarcinoma stomach-a case report. Aust Med J 2013;6(10):515-519.
| How to Cite This Article: Seetharamaiah VB, Sunil B, Padmanabha MK, Sparsha N. Carcinoma of Unknown Primary Mimicking Multiple Myeloma. Journal of Orthopaedic Case Reports 2017 Mar-Apr;7(2):44-47. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com





