 |
| While some people, including supermodel Gisele Bundchen, believe sunscreen is dangerous (she declared “I cannot put that poison on my body”) experts such as The Skin Cancer Foundation and the American Academy of Dermatology—and even Cosmopolitan magazine—disagree with her and other skeptics. |
A large, randomized controlled trial examined the effect of daily sunscreen use on the development of skin cancers. Researchers followed 1621 Australians from 1992-2006. From 1992-1996, participants were randomly placed in a group and instructed to either use the study-provided broad spectrum SPF 16 sunscreen daily on face, arms, neck and hands, or to continue personal discretionary use of sunscreen. At the 2004 follow up, researchers noted that the daily sunscreen use group had a 35% rate reduction in the incidence of SCC (considering all SCCs that appeared throughout the entire study). However, the incidence of BCC was not statistically different between the two groups. More recent studies corroborate these results.
 |
| US Senator and 2008 Republican Presidential Candidate John McCain has had multiple melanomas removed. Other political figures have battled skin cancer, including former Presidents Jimmy Carter (metastatic melanoma) and Bill Clinton (BCC), and former First Lady Laura Bush (SCC). |
In 2006,
researchers followed up again, this time looking for melanoma. The overall
incidence rate of melanoma was 50% less in the sunscreen intervention group
than the discretionary use group (out of approximately 800 people in each
group, 11 people in sunscreen group and 22 in the control group developed melanoma).
It should be noted that these results had borderline statistical significance,
with a P value of 0.051 (P = 0.05 is the accepted cutoff for significance).
This essentially translates to a 5.1% probability of these findings being due
to chance, rather than to the actual sunscreen intervention. Also, there was a
73% lower rate of invasive melanoma in the sunscreen group. Although there was
no significant difference in number of melanomas diagnosed at the prescribed
intervention sites, it is possible that sunscreen use reduced the risk, as
participants in the sunscreen intervention group reported more frequent use of
sunscreen over the whole body after the intervention terminated.
Although
these results are not the most compelling, they nonetheless point to a
protective role of sunscreen. Many factors may contribute to a less than
straightforward outcome. First, the sunscreen intervention was in adults and
lasted 4.5 years. Melanoma and BCC are thought to result from both long term sun
exposure and intense, intermittent episodes (sunburns), whereas SCC is mainly
caused by cumulative UV exposure (both natural and indoor tanning bed).
Furthermore, blistering childhood sunburns are a risk factor for melanoma. One study
that examined sunscreen use in children found a significant protective benefit.
Regular use (applied any time sun exposure would exceed 30 min) of a
broad-spectrum SPF 30 sunscreen over a 3-year period resulted in significantly
fewer newly developed moles, the number of which is a risk factor for melanoma.
Second, participants
in the non-sunscreen intervention group continued their discretionary use of
sunscreen. No trial in humans could ever prohibit sunscreen use or provide a
placebo for ethical reasons. Therefore, perfectly delineating the protective
effect of sunscreen is difficult.
Many questionnaire-based
studies that rely on participants’ memory of sunscreen use suffer from recall
bias. Some of these studies showed no benefit of sunscreen for melanoma
prevention but memory limits the reliability of these results. The bottom line
is that sunscreen protects from UV radiation, a known human
carcinogen.
UV radiation is implicated in up to 90% of nonmelanoma skin cancers, squamous cell carcinoma (SCC) and basal cell carcinoma (BCC). Mutations consistent with UV radiation were also found in the genomes of melanoma tumors; UV radiation is thought to be responsible for the majority of melanoma. Whereas SCC and BCC are more frequent, melanoma is more often fatal. While UV radiation is the single most important risk factor for skin cancer, it’s worth noting that it is not responsible for all skin cancers. Aside from environmental carcinogens, cancer can arise due to a person’s genetics (familial effect) or random mutations.
 |
| Acral melanoma is a type of skin cancer not caused by UV radiation and is genetically distinct from UV-induced cutaneous malignant melanoma. Bob Marley’s acral melanoma metastasized and ultimately claimed his life. |
UVA
radiation primarily damages the components of skin cells by generating reactive
oxygen species, or ROS. These highly active molecules can cause single-strand
breaks in the DNA or crosslink DNA to protein, resulting in mutations or
improper functioning. Both UVA and UVB can cause a more significant type of DNA
damage called pyrimidine dimers, where two adjacent pyrimidine nucleotides (the
“C” and “T” of DNA; the “A” and “G” are purines) fuse together. Because the
higher energy UVB is absorbed directly by DNA, UVB can cause other
modifications that compromise the integrity of DNA, leading to instability of
the genetic code.
Indeed,
the cell has repair mechanisms to fix pyrimidine dimers and other errors, but
sometimes the very genes encoding the repair mechanisms are mutated. UV-induced
DNA damage can result in highly characteristic mutations in critical genes, for
example in the tumor suppressor gene p53. As the “guardian of the genome”, the
p53 protein is involved in directing the repair of mutations and guiding the
cell through its controlled death pathway, called apoptosis. Mutations in p53
are thought to be among the first steps in development of non-melanoma skin
cancer. Formation of malignant melanoma is more complicated and not fully
understood.
 |
| Yes, p53 has its own superhero persona. That’s how cool (and significant) it is. Image by Susanne Harris. |
Cells that carry mutations in p53 proliferate uncontrollably, a hallmark of cancer. In some cases, the immune system will recognize malignant cells as a threat and effectively eliminate them. However, UV radiation is also known to suppress the immune system by at least two mechanisms. One is by diminishing the production of antigen-presenting cells, which engulf foreign-looking cells and display an alert to activate the immune system). The other is by inducing the production of an immune suppressive cytokine, interleukin-10. Additionally, some skin cancer cells display proteins on their surface that prevent the immune cells from killing them. Thus, in addition to mutations in key genes, immune suppression and immune evasion contribute to the development of skin cancer.
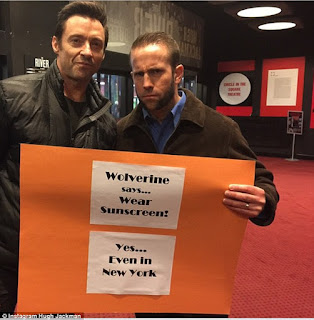 |
| Even the mutant Wolverine wears sunscreen! In this Instagram post, Hugh Jackman urged his fans to use sunscreen. He became a fervent sunscreen proponent after having a BCC removed from his nose. |
Contributed by: Julia van Rensburg, Ph.D.
Follow Julia on Twitter.
van der Pols JC, Williams GM, Pandeya N, Logan V, & Green AC (2006). Prolonged prevention of squamous cell carcinoma of the skin by regular sunscreen use. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology, 15 (12), 2546-8 PMID: 17132769
Lee TK, Rivers JK, & Gallagher RP (2005). Site-specific protective effect of broad-spectrum sunscreen on nevus development among white schoolchildren in a randomized trial. Journal of the American Academy of Dermatology, 52 (5), 786-92 PMID: 15858467
Koh HK, Geller AC, Miller DR, Grossbart TA, & Lew RA (1996). Prevention and early detection strategies for melanoma and skin cancer. Current status. Archives of dermatology, 132 (4), 436-43 PMID: 8629848
Leiter U, & Garbe C (2008). Epidemiology of melanoma and nonmelanoma skin cancer--the role of sunlight. Advances in experimental medicine and biology, 624, 89-103 PMID: 18348450
Brenner M, & Hearing VJ (2008). The protective role of melanin against UV damage in human skin. Photochemistry and photobiology, 84 (3), 539-49 PMID: 18435612

Thanks for sharing useful information with us. Yes, you are right that everybody is free to wear sunscreen
ReplyDelete