Scientists believe they have made a major advance in the quest to find an effective treatment for type 1 diabetes.
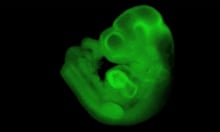
Using human embryonic stem cells as a starting point, they have for the first time been able to create human insulin-producing beta cells equivalent in almost every way to normally functioning beta cells in the kind of large quantities needed for cell transplantation and pharmaceutical purposes.
Doug Melton, Xander University Professor at Harvard University, who led the work, said he hopes to have human transplantation trials using the cells under way within a few years.
The stem cell-derived beta cells are currently undergoing trials in animal models, including non-human primates.
Prof Melton, who is also co-director of the Harvard Stem Cell Institute, said a device being tested had so far protected beta cells implanted in mice from immune attack for many months.
“[While] there have been previous reports of other labs deriving beta cell types from stem cells, no other group has produced mature beta cells as suitable for use in patients,” he said.
“The biggest hurdle has been to get to glucose-sensing, insulin-secreting beta cells, and that’s what our group has done.
“We are now just one pre-clinical step away from the finish line.”
Beta cell transplantation as a treatment for diabetes is still essentially experimental. It uses cells from cadavers, requires the use of powerful immunosuppressive drugs and has been available to only a very small number of patients.
Professor Elaine Fuchs, of Rockefeller University, described the findings as “one of the most important advances to date in the stem cell field”.
“For decades, researchers have tried to generate human pancreatic beta cells that could be cultured and passaged long term under conditions where they produce insulin. [Professor] Melton and his colleagues have now overcome this hurdle and opened the door for drug discovery and transplantation therapy in diabetes,” she said.
About 10% of all diabetes is type 1, but it is the most common type of childhood diabetes.
It is an autoimmune condition that causes the pancreas to stop producing insulin – the hormone that regulates blood glucose levels. If the amount of glucose in the blood is too high it can seriously damage the body’s organs over time.
A report on the work is published in the journal Cell.




Comments (…)
Sign in or create your Guardian account to join the discussion